Roundtable #13: Healthcare Worker Burnout and Brain Health
In October, the Business Collaborative for Brain Health convened to discuss brain health through the lens of the healthcare workforce and healthcare worker burnout as a result of the pandemic.
Speakers in the roundtable included:
● Jeannie Southworth Nigam, Research Psychologist; Co-Coordinator, Healthy Work Design and Well-being at National Institute for Occupational Safety and Health (NIOSH)
● Lisa Gables, Chief Executive Officer at American Academy of Physician Associates
Healthcare Worker Burnout and Brain Health: It Begins with Stress
Jeannie Nigam opened the discussion by defining stress as “the feeling that arises when external demands exceed an individual’s resources or abilities.” She noted that everyone experiences stress differently, depending on available resources, coping strategies, personal circumstances and workplace support. Common symptoms of stress include irritability, anxiety, lack of motivation, fatigue and feeling overwhelmed among others. She explained how chronic, unaddressed stress can lead to other health issues, reinforcing the importance of managing stress in the workplace.
Nigam elaborated on workplace stressors, explaining that factors at the organizational level such as job design, workload, and workplace safety significantly affect stress. Interpersonal and psychosocial factors also play a role, impacting how well workers get along, the level of support and supervision available, and the presence of any harassment or discrimination. Exposure to such stressors impacts not only physical health but also mental well-being and behavior.
The Impact of COVID-19 on the Healthcare Workforce
Nigam continued by explaining how the COVID-19 pandemic had a substantial negative impact on the workforce, with workers suddenly adapting to changes in when, where and how they worked, almost overnight. Many were balancing childcare or eldercare responsibilities while trying to keep themselves and their families safe. Essential workers, in particular, faced heightened stress, with one in four reporting a mental health disorder in 2021, according to the American Psychological Association (APA).
(Featured image from NIOSH)
Healthcare workers, already dealing with high-stress levels before the pandemic, faced additional challenges during this period. These included heightened exposure risks, resource shortages, physical and emotional exhaustion, harassment and isolation from loved ones. Many reported lacking time for self-care and facing stigma around seeking mental health support.
It was for these factors that Nigam and the team at NIOSH studied the stress experienced by healthcare workers. See: MMWR Vital Signs
Nigam shared some of the findings from the study, noting that healthcare workers reported worse outcomes in 2022 than in 2018. In addition, the percentage of healthcare workers experiencing burnout rose significantly, whereas it stayed relatively stable for other essential workers and increased only slightly for all other workers. Notably, turnover retention, an incredibly important factor for the health industry at large as well as other employers, increased markedly for health workers, while decreasing across other industries.
Healthcare workers also had to deal with varying levels of harassment. Among healthcare workers who faced harassment:
● 85% reported feelings of anxiety
● 60% reported symptoms of depression
● 81% reported symptoms of burnout
The study also highlighted deteriorating working conditions, with a notable decline in trust in management and a decrease in workplace support for productivity. Given these findings, Nigam emphasized how data-driven insights can help employers better understand the link between workplace support and how it impacts employee brain health and well-being.
Following the release of their study, NIOSH launched a national campaign, Impact Well-Being, promoting primary prevention strategies like participatory decision-making, supportive supervision and psychological safety. Additionally, they introduced a burnout prevention training program for healthcare supervisors, focusing on improving workplace conditions to support mental health, rather than placing the burden of resilience solely on workers.
The Solution to the Healthcare Worker Crisis
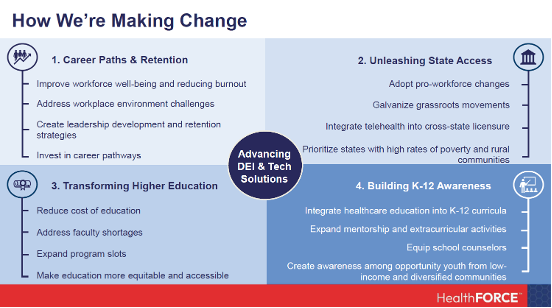
Lisa Gables then introduced HealthFORCE, a national alliance of leaders dedicated to addressing the root causes of our nation’s healthcare workforce crisis. The goal of HealthFORCE is to take a comprehensive look at the workforce crisis and its impact on mental health and burnout. Gables shared how this shortage affects everyone: patients, the public and the workforce, itself. The lack of healthcare providers has created areas across the country with little or no access to care.
Gables pointed to statistics projecting a shortage of 3.2 million healthcare workers by 2026, emphasizing that unless we act now, this problem isn’t going away. She explained how this can impact public perceptions of the healthcare system citing a 2023 Harris Poll conducted by the American Psychological Association (APA) which found that 73% of Americans feel the healthcare system isn’t meeting their needs.
(Featured image from the American Academy of Physician Associates)
Long wait times and complex care coordination are leading people to skip their own care due to the system's inefficiencies. This situation affects all employers—not just in healthcare—as employee productivity and attendance are impacted by these gaps in care.
The aging population only adds to this urgency, explained Gables. The number of people over 65, who are the highest users of healthcare, is growing substantially. We're also seeing shifts in healthcare delivery, with telemedicine and convenient care. However, these innovations can’t fully compensate for the healthcare workforce shortages. And even with telemedicine, Gables stressed how we still need people to conduct visits, and that technology alone can't solve these gaps.
She explained that addressing this problem requires a multi-faceted approach. First, we need to engage people in healthcare career pathways from an early age, creating awareness of healthcare roles beyond doctors and nurses. Programs targeted at K-12 students can help make healthcare careers visible and appealing, expanding options for students long before they consider career paths.
Finally, Gables shared how HealthFORCE is tackling clinician burnout directly, with a focus on career satisfaction and mobility to help retain staff in the system. Their goal is to reduce burnout by ensuring adequate staffing and creating pathways for career growth and satisfaction.
HealthFORCE is unique in its holistic, cross-sector approach. The national alliance includes a wide range of stakeholders—businesses, advocacy groups, and healthcare organizations — working together on this issue. With over 100 volunteers and a steering committee that includes representatives from Amazon and Georgetown University, their mission is broad and inclusive, addressing shortages across all provider types and disease states. HealthFORCE working groups are addressing every level of the problem, from K-12 engagement to workforce policies, all with an emphasis on diversity, equity and technology.
(Featured image from the American Academy of Physician Associates)
Gables forecasted that if HealthFORCE is successful, patients will receive timely care, providers will experience reduced burnout, employers will be adequately staffed, and society, as a whole, will benefit.
Business Collaborative for Brain Health Updates
Kelly O’Brien, Vice President of Prevention, closed the meeting with updates and data on the Brain Health Best Practice Score and the importance of research to understand the correlation between employer scores and employee mental health outcomes, proposing a research work group to explore further insights.
She emphasized the growing momentum around brain health awareness in the workplace, citing recent media coverage and company inquiries into the Scorecard. O’Brien closed the meeting by outlining future plans for November including the development of a resource hub with practical tools for employers.
The Business Collaborative for Brain Health (BCBH) is a collaborative of private sector partners developing innovative solutions to cognitive health throughout the lifespan. The Collaborative hosts regular roundtables to learn from experts and stakeholders and refine the work. If you’re interested in attending or participating in a roundtable discussion or want to learn more about how you can get involved with the Collaborative visit: https://businessforbrainhealth.org/