Roundtable Brief #1: The Case for Private Sector Engagement in Brain Health
About the Business Collaborative for Brain Health
The Business Collaborative for Brain Health is a group of private sector partners developing innovative solutions to optimize cognitive health throughout the lifespan. The Collaborative’s mission is to build brain health capital by advancing measurably effective brain healthy workplaces, communities, and product and service innovations.
The Collaborative’s premise is that promoting brain health is essential to growing the U.S. our economy, strengthening national security, and improving health and well-being. Our nation relies on brainpower more than ever before to solve critical challenges and drive innovation. Profound demographic and technological shifts have resulted not only in labor and skill shortages but also in an older workforce in an increasingly knowledge-based economy. Brain health and performance must be a national priority if we are to thrive. Promoting brain health and mitigating cognitive decline offers us an opportunity to build prosperous, more inclusive, multigenerational communities and workplaces—if we can ensure that we are not just living longer but living healthier longer—both physically and cognitively.
About the Roundtable Series
The Business Collaborative for Brain Health is engaging global business leaders and experts in roundtable discussions around key issues to inform and advance meaningful action and measurable results. Each roundtable is summarized in a brief for Collaborative members and the public.
The May 2023 roundtable, “The Case for Private Sector Engagement,” asked discussants to address the available data to help demonstrate the relationship of brain healthy aging to the economy, to inequalities, and to business objectives. Moderated by Anne Tumlinson, Founder and CEO of ATI Advisory, the panel featured Shayla Smith, from the Institute for Health Metrics and Evaluation (IHME); Dr. Stephen White, with the Center for BrainHealth® at the University of Texas at Dallas; Dr. Lisa D'Ambrosio, representing the MIT AgeLab; and Michael Acker, with Sharecare Inc. An additional roundtable, “Connecting the Dots for Impact,” asked speakers to address ways that employers could apply current knowledge to advance brain health in their own organizations and in the nation at large, articulating possible next steps. Some of this related discussion, led by Lisa Gables, of the American Academy of Physician Assistants (AAPA), has been incorporated into this brief. Participants included Thomas Seoh, with Kinexum; Rajiv Ahuja, from the Milken Institute; and Rich Beatty, with CMG Consulting.
Scope of the Problem
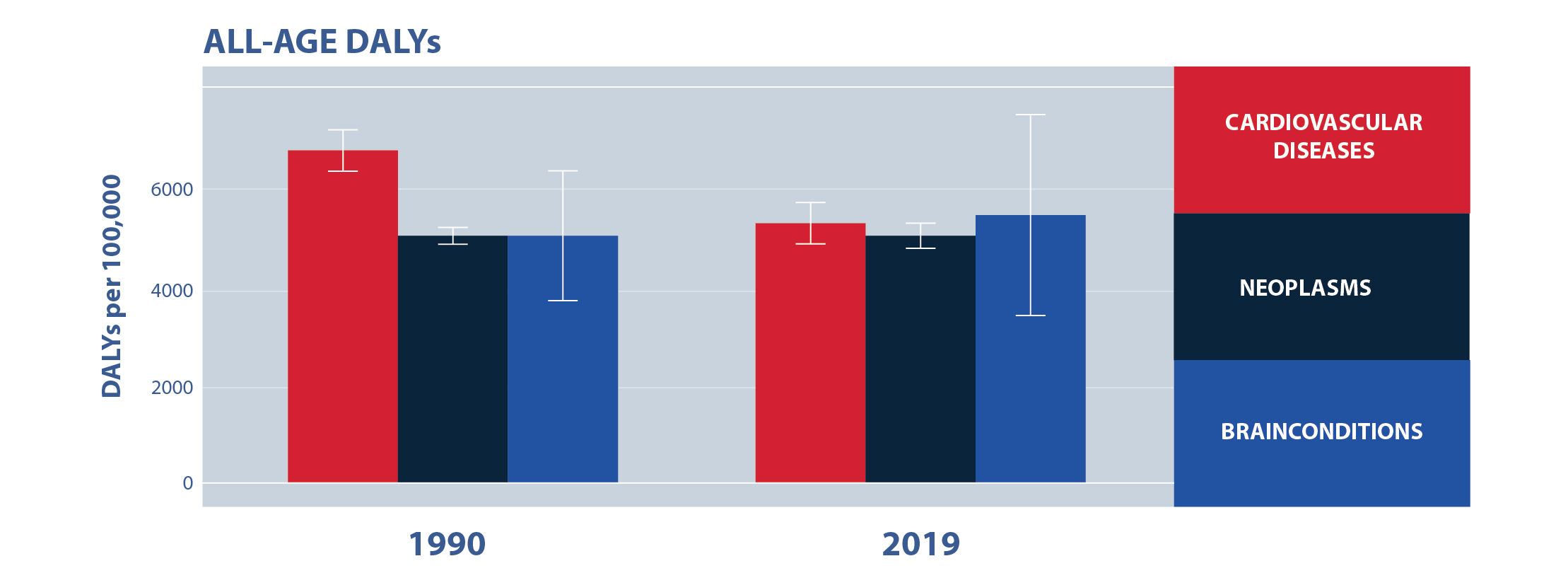
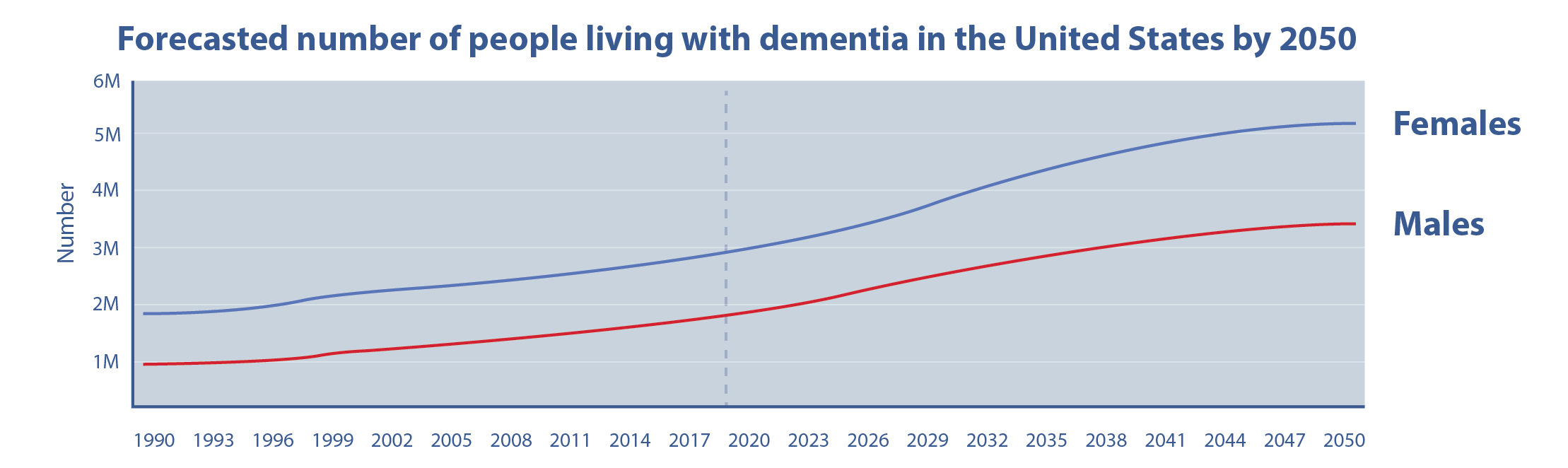
IHME maintains one of the largest datasets in the world accurately measuring the impacts of brain health. It shows that total health loss due to brain disorders in the United States is on par with cardiovascular diseases and cancer and that the burden of brain disorders is increasing relative to other disorders. Dementia is on the rise. In the United States, there are approximately 4.9 million people living with dementia, 78 percent more than in 1990, a higher rate of increase than that among people living with anxiety and depression.
By 2050, an additional 50 million people in the U.S. will be between the ages of 65 and 79, and dementia cases are expected to double.
IHME’s Shayla Smith emphasized that brain disorders affect people of all ages, including those in the current workforce. As populations grow and age, a data-driven approach is necessary to understand areas where employers should be prioritizing resources and developing policy to improve and maintain the health and well-being of their employees. IHME’s Brain Health Initiative was established to provide effective evidence for decision-makers and communicate the urgency of brain disorders around the world. The initiative analyzes a wide range of sources for brain disorder data, including neurological, cerebral, vascular, and mental health disorders. Through the utilization of metrics relating to the global burden of disease, IHME can determine the prevalence of brain disorders on an international level and use this analysis to make geographic and hyperlocal estimations about brain health. Ms. Smith elaborated, “the . . . process of understanding the data, understanding the size of the problem, what the trends are, developing an action plan, an intervention strategy, and then analyzing those results” could give consumers the brain health security they deserve.
The MIT AgeLab, a multidisciplinary research program devoted to studying the multifaceted impacts and outcomes of aging, focuses on the areas of retirement, well-being, home logistics, and transportation to test and study gaps in brain health knowledge. Research Scientist Dr. Lisa D’Ambrosio reported that separate from the burden for those with impaired brain health, the burden of caregiving, according to an AgeLab study, represents “$33.6 billion in lost productivity related to caregivers in the workplaces, which is about $2,000 for employers per full-time employee.”
The Brain Health Project at the University of Texas is the world’s first multidimensional measure of the brain’s actual performance. It started two years ago, and the goal is to track 120,000 people over the course of 10 years to understand what works to improve brain fitness. More than 27,000 people from all 50 U.S. states and 60 other countries are already participating. Early results demonstrate that brain health is not only measurable but in fact improvable.
Sharecare, a publicly traded company founded by Jeff Arnold (the former founder and current President and CEO of WebMD), works across the entire ecosystem of healthcare, to help nearly 10 million employees, plan members, and patients across the country better understand their health and optimize their healthcare benefits. Michael Acker explained that Sharecare has developed a well-being score incorporating demographic characteristics, job codes, and even employee geographical location (from region to city to neighborhood). This information helps employers see the importance of factors such as commute time, community circumstances, and anxiety levels to their employees' well-being. Sharecare is using these data to help build public-private partnerships in neighborhoods that have been historically marginalized and left behind. Sharecare has also created an evidence-based measurement methodology around well-being that incorporates predictive analytics to tell the employer the cost of neglecting employee well-being.
Information Gaps
Despite the volume of data to track and measure the prevalence and impact of brain disorders and the economic costs of impaired brain performance, data and knowledge gaps still exist. IHME’s Shayla Smith noted that these gaps generally revolve around factors like community engagement, business insights, and effective interventions. For example, even though 95 percent of people believe it is possible to improve brain performance and function, only 3 in 10 know how.
Michael Acker added that employers still don’t know what things will and won’t work in regard to brain health initiatives. The journey for an individual with respect to health and healthcare is fragmented, it's hard, it's full of disinformation, and it's a confusing process.
Lisa D’Ambrosio added that despite the data on productivity losses related to employee caregiving responsibilities, employers are largely unaware of the prevalence in their own workforce and therefore cannot support employed caregivers with the proper resources.
Since the lack of brain health care is largely a systemic issue, the brain health continuum differs for many businesses. “Some employers are thinking in terms of stress and anxiety, while others are thinking in terms of home care and caregiving,” observed Mr. Acker. Clearly, companies are starting take brain health measures; nonetheless, the private sector must develop initiatives that are relevant for their employees and rewarding for their company. There are many resources available to employees, but receptivity, uptake, and engagement is low.
Case for Private Sector Engagement
There is a return on investment (ROI) to employers who address brain health, said Dr. Steven White with the Center for Brain Health (CBH) at the University of Texas. CBH’s research and measurable findings on brain training demonstrated it can return the lost 15-18 percent of workplace efficiency, yield valuable ROI, and increase worker engagement. He emphasized that a dollar spent in health is 80 percent more efficient than a dollar spent trying to treat disease and it is critical that we shift the mindset around brain health to be more proactive.
Dr. D’Ambrosio added that this is an opportunity for us not only to redefine how we think about brain health but also think about who the new markets and new consumers are. Addressing brain health presents an opportunity for companies to redefine how they're engaging and interacting with their employees and also what kinds of new products and services they should be thinking about to supply this market.
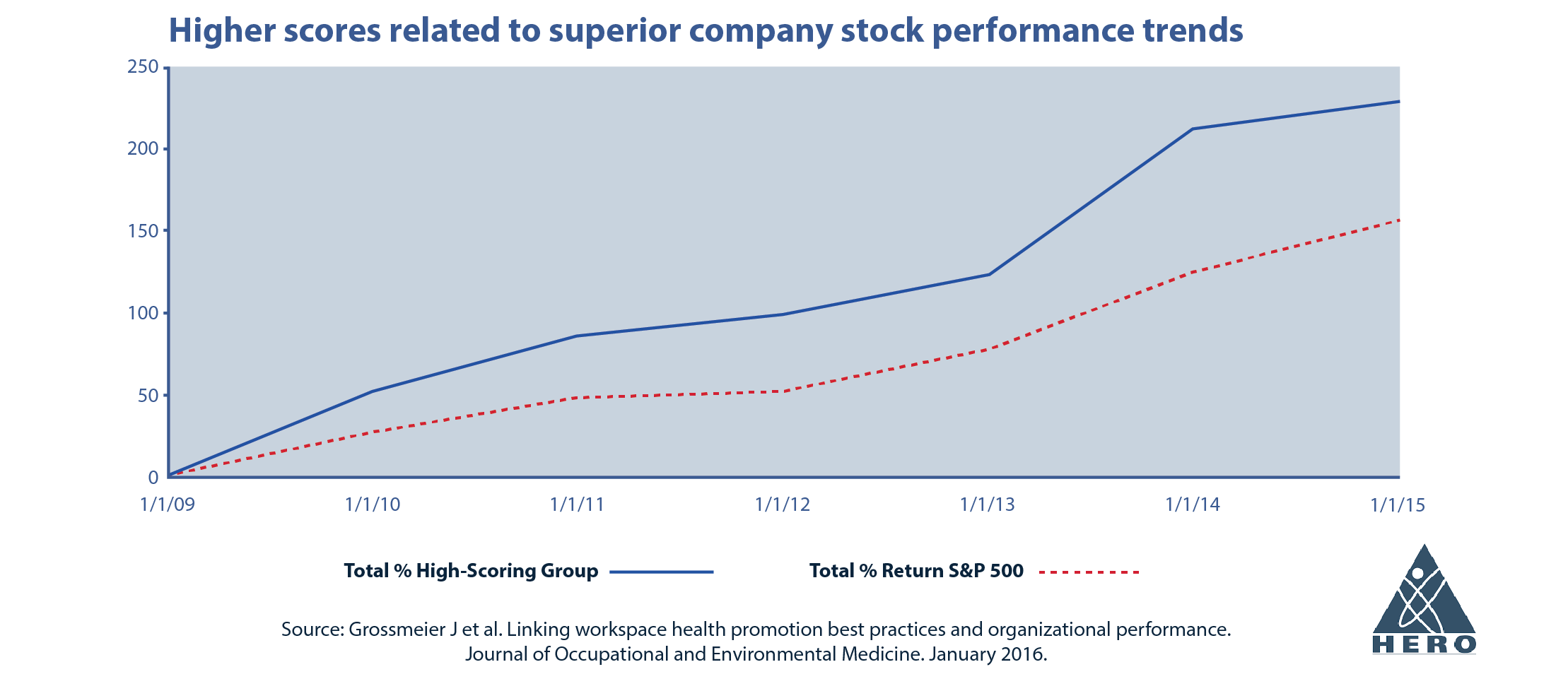
The Health Enhancement Research Organization (HERO Health) is finding a relationship between well-being and stock market performance. Dedicated to connecting science and practice to demonstrate the value of health and well-being in workplace ecosystems, HERO’s work began in 1998 with a landmark study that demonstrated lifestyle and behavior connected to healthcare costs through a multi-employer dataset.
As a result of preliminary findings and progressive data, the “HERO Scorecard” was launched, in collaboration with Mercer, as a free, online tool to assess workplace health promotion and provide businesses a way to “score” their practices. Karen Mosley, President of HERO Health, stated that the “HERO Scorecard high performers portfolio showed a 235 percent appreciation versus the S&P 500.[i]” These findings reveal that it may be possible to invest in stocks of companies that have adopted best practices in health and well-being. Further, awards programs and incentives for high-scoring businesses can serve as a motivator for superior health outcomes and business results.
Due to the success of the Hero Scorecard, new categories like mental and emotional well-being, social determinants of health, and DEI efforts are being implemented into the survey to further explore data gaps. Additionally, HERO leaders believe that a “brain health best practice score” would foster substantial improvements in productivity and engagement across the business sector.
Addressing brain health may also be a way to help mitigate the current workforce shortage challenge in the U.S. Keeping people healthier and, in the workforce, longer, including older adults who might otherwise retire is an opportunity, said Lock.
Conclusion
Anne Tumlinson with ATI summarized some of the key points raised by speakers: It essential that employers and businesses incorporate policies that support brain health because brain disorders are costly to both private health insurers and employers. Because promoting brain health is essential to growing our economy, strengthening national security, and improving overall health and well-being, the C-Suite as well as human resource departments need to address this challenge. Although we have significant data about the toll poor brain health takes on human well-being longevity, and the national economy, we need more and better data to help employers implement strategies that boost their return on investment. As Michael Acker put it, people with high well-being cost less and perform better. It will be important for businesses to come to the table and lead on this issue, not simply react.
May, 2023
The Business Collaborative for Brain Health is a group of private sector partners developing innovative solutions to optimize cognitive health throughout the lifespan. The Collaborative’s mission is to build brain health capital by advancing measurably effective brain healthy workplaces, communities, and product and service innovations.
Founding Partner
[i] Grossmeier J et al. Linking workplace health promotion best practices and organizational performance. Journal of Occupational and Environmental Medicine. January 2016.